Glaucoma Treatment Options 2026: A Comprehensive Guide
Glaucoma care is changing rapidly, combining long established therapies with newer technologies that aim to protect sight more effectively. This guide for readers worldwide explains the main types and causes of glaucoma, outlines current and emerging treatment options, and highlights practical lifestyle adjustments that can support eye health and treatment success in everyday life.
Glaucoma Treatment Options 2026: A Comprehensive Guide
By 2026, glaucoma care brings together proven pressure lowering therapies and innovative tools designed to preserve vision for longer. Understanding how glaucoma develops, what treatment options exist now, and which advances are on the horizon can make discussions with eye specialists clearer and more productive. This guide looks at glaucoma types and causes, current therapies, research directions, treatment risks, and realistic lifestyle adjustments that support long term eye health.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Understanding glaucoma: types and causes
Glaucoma is a group of eye conditions that damage the optic nerve, the structure that sends visual information from the eye to the brain. In many people, this damage is linked to increased pressure inside the eye, called intraocular pressure. Fluid inside the eye is constantly produced and drained; when the drainage system does not work efficiently, pressure can rise and gradually harm the optic nerve.
The most common form worldwide is primary open angle glaucoma. In this type, the drainage angle between the cornea and iris appears open, but the microscopic outflow channels do not function normally. Angle closure glaucoma happens when the drainage angle becomes blocked, often quickly, and can cause sudden pain and blurred vision. Other forms include normal tension glaucoma, where optic nerve damage occurs despite pressure readings within the typical range, and secondary glaucomas caused by eye injuries, inflammation, advanced cataract, or long term use of steroid medications.
Genetics, age, family history, ethnicity, and conditions such as diabetes or high blood pressure can influence glaucoma risk. Not everyone with elevated eye pressure develops glaucoma, and some people with modest pressure levels still experience damage. This complexity is one reason regular comprehensive eye examinations and optic nerve evaluations are so important.
Current treatment options for glaucoma
The main aim of glaucoma treatment is to lower intraocular pressure to a target range that is safer for the optic nerve. Treatment plans are tailored to the individual, taking into account the type and stage of glaucoma, baseline pressure, age, and other health conditions. In many cases, therapy begins with medicated eye drops.
Eye drops include several groups of medications. Prostaglandin analogs improve fluid outflow and are often prescribed once daily. Beta blockers reduce fluid production in the eye, while carbonic anhydrase inhibitors and alpha agonists can either decrease production, increase outflow, or both. Some patients use combination drops that contain more than one active ingredient, which can simplify routines. Oral medications are used less commonly today but may be added when drops and procedures are not enough on their own.
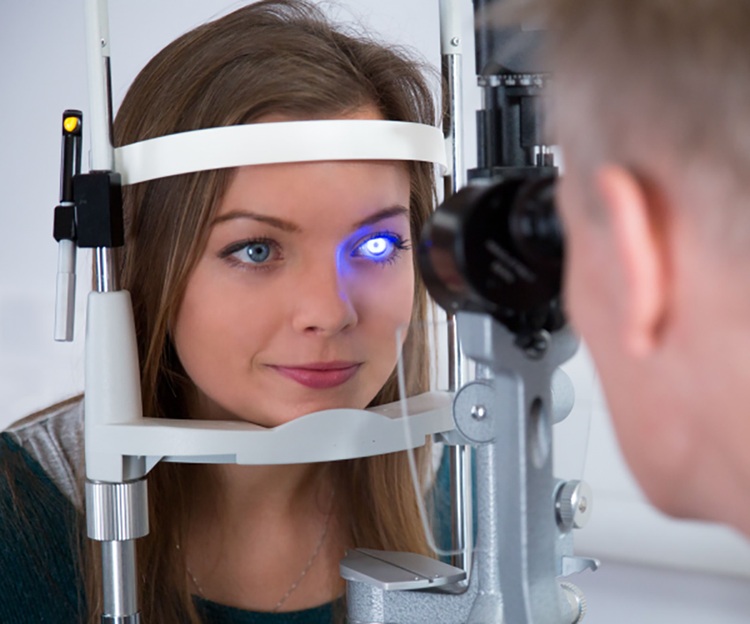
Laser treatments are another established option. Selective laser trabeculoplasty targets the drainage tissues in open angle glaucoma and can reduce pressure without making an incision. For angle closure glaucoma, laser iridotomy creates a tiny opening in the iris to improve fluid movement between eye chambers. Laser cyclophotocoagulation, often reserved for more advanced or complex cases, reduces the eye tissue that produces fluid.
When medications and laser treatment do not adequately control glaucoma or cannot be tolerated, surgery may be recommended. Traditional procedures such as trabeculectomy create a new drainage pathway for fluid to leave the eye, while drainage devices use tiny tubes and plates to divert fluid. In the past decade, minimally invasive glaucoma surgeries, often called MIGS, have been developed to lower pressure with smaller incisions and typically faster recovery. Surgeons choose among these approaches based on disease severity, eye anatomy, and previous surgeries.
Innovative research and future directions in glaucoma care
Glaucoma research is active worldwide and focuses on more than simply lowering eye pressure. One major area involves sustained release drug delivery systems. Instead of daily drops, tiny implants, punctal plugs, or long acting injections may release medication slowly over weeks or months. These strategies aim to reduce the burden of remembering multiple daily doses and to ensure more consistent drug levels on the eye surface.
Another promising direction is neuroprotection and optic nerve support. Researchers are studying medications and biological agents that may help protect nerve cells from damage, even when pressure is reasonably controlled. Gene based therapies seek to modify the behavior of cells involved in fluid drainage or to support the survival of retinal ganglion cells. While many of these approaches are still in clinical trials, they illustrate a shift toward protecting the optic nerve more directly.
Digital technologies are also shaping the future of glaucoma care. Remote monitoring tools, home tonometry devices, and artificial intelligence supported analysis of optic nerve images may allow earlier detection of change and more precise adjustment of treatment. As these tools mature, they could support closer follow up, especially for people who find it hard to attend frequent clinic visits.
Managing risks associated with glaucoma treatments
Every glaucoma treatment, from eye drops to surgery, carries potential risks or side effects. Common issues with drops include redness, burning, dry eye, or allergic reactions. Some medications, such as beta blockers, can affect heart rate or breathing in susceptible individuals. For this reason, people with heart or lung disease need careful assessment and ongoing monitoring when using these drugs.
Laser treatments are generally safe but may cause temporary inflammation, blurred vision, or pressure spikes shortly after the procedure. Surgical procedures like trabeculectomy and drainage devices bring higher risks, including infection, bleeding, scarring of the drainage site, or pressure dropping too low. Over time, surgery can also influence the development or progression of cataract in the operated eye.
Managing these risks starts with open communication. Patients should inform their eye specialist about all medications, allergies, and existing health conditions, and report new symptoms promptly. It is important not to stop glaucoma medication suddenly without medical advice, even if side effects occur, because uncontrolled pressure can lead to permanent vision loss. Regular follow up visits, visual field tests, and optic nerve imaging help clinicians adjust treatment before serious damage develops.
Expert insights on lifestyle adjustments for glaucoma patients
Lifestyle cannot replace medical or surgical treatment for glaucoma, but it can support eye health and treatment success. Many specialists encourage regular, moderate physical activity such as walking, gentle cycling, or swimming, which can benefit overall circulation and general health. Very heavy weight lifting or activities that involve breath holding for long periods may temporarily raise eye pressure, so they are sometimes discouraged for people with advanced disease.
Sleeping position can also matter. Some studies suggest that lying consistently on the same side or using very low pillows might slightly increase pressure in the eye closest to the pillow. Using a slightly elevated head position and discussing concerns with an eye care professional can be helpful. People with sleep apnea should mention it to their ophthalmologist, as untreated sleep apnea may influence optic nerve health in some individuals.
Practical adjustments around the home can reduce the impact of glaucoma related vision changes. Better lighting, high contrast markings on steps, and avoiding clutter can reduce the risk of falls. Organizing medications in a weekly pillbox or using reminder apps may help with complex drop schedules. Emotional wellbeing is also important; speaking with counsellors, support groups, or trusted friends and family can help people adjust to the long term nature of glaucoma management.
In summary, glaucoma treatment in 2026 combines established pressure lowering strategies with emerging drug delivery systems, nerve protecting approaches, and digital tools. Understanding the type of glaucoma, the goals and risks of each therapy, and the role of practical lifestyle changes can support more confident decisions and closer collaboration with eye care professionals over the long term.




